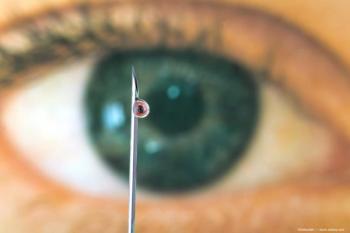
Retina Society 2024: Differential artery-vein analysis improves OCTA performance for AI classification of diabetic retinopathy
Jennifer Lim, MD, FARVO, FASRS, discusses her presentation on differential artery-vein analysis and how it improves OCTA performance for AI classification of diabetic retinopathy at the annual Retina Society meeting being held this year in Lisbon, Portugal.
Jennifer Lim, MD, FARVO, FASRS, sat down with David Hutton of Ophthalmology Times to discuss her presentation on differential artery-vein analysis and how it improves OCTA performance for AI classification of diabetic retinopathy at the annual Retina Society meeting being held this year in Lisbon, Portugal.
Video Transcript:
Editor's note: The below transcript has been lightly edited for clarity.
David Hutton:
I'm David Hutton of Ophthalmology Times. The Retina Society is holding its 57th annual scientific meeting in Lisbon, Portugal. At the meeting, Dr Jennifer Lim made a presentation titled Differential Artery-Vein Analysis Improves OCTA Performance For Artificial Intelligence Classification of Diabetic Retinopathy. Dr Lim, thank you so much for joining us today. First, tell us a little bit about your presentation.
Jennifer Lim, MD, FARVO, FASRS:
It's my pleasure to be here today with you David. At my presentation, we discuss the use of artificial intelligence as applied to OCTA and specifically to artery-vein differentiation, to try to distinguish different types of nonproliferative diabetic retinopathy from each other and also from control eyes. And basically what we did is we analyzed the vessels with regards to whether they were from arteries or veins. And then ran several parameter checks on these vessels, if you will, and compared them. And what we found out was because certain characteristics, such as, for example, blood vessel caliber, change differently between arteries and veins. When we analyze it separately, we can actually get higher levels of differences between the different stages of retinopathy. So for example, as retinopathy progresses, the arteries become narrower. And as it progresses, sometimes the veins initially increase in size in terms of their caliber as the change. So if you then look at the ratio of artery to veins, this becomes even more sensitive than just looking at the caliber overall. Because obviously, if it's increasing, say for veins, but decreasing for arteries, the overall value may not change. Yet if you distinguish it between the types of vessels, you will see a change, and that change could be powerful and help you distinguish the levels of diabetic retinopathy from each other and from control eyes.
David Hutton:
What impact does the improved artery vein differentiation have on the accuracy and reliability of AI models and predicting different stages of diabetic retinopathy.
Jennifer Lim, MD, FARVO, FASRS:
You know, that's a great question. And when we looked at the various variables that we looked at, the improvement in the accuracy could range anywhere from 2% up to 16%. And on average, the improvement in accuracy was 9%. So this is a substantial boost when trying to determine, is this level of retinopathy moderate, or is it mild retinopathy, or is it severe retinopathy? And it can be very useful.
David Hutton:
Were there any particular patterns or biomarkers identified in the artery vein analysis that maybe were previously overlooked in OCTA imaging for diabetic retinopathy?
Jennifer Lim, MD, FARVO, FASRS:
Well, you know, I think it goes back to the same question, and it's basically that–Yes, there are some variables, such as caliber, which, if you look at them separately, can be very useful. As well as tortuosity of vessels, which can again be more useful, say, for veins and for arteries. And these differences may not have been used before, because they were looked at in the aggregate. And so when you separate them out, looking again at arteries or looking at veins, some of these biomarkers may become significant as compared to the aggregate biomarker evaluation.
David Hutton:
And ultimately, what can all this mean for retina specialists and the patients they treat?
Jennifer Lim, MD, FARVO, FASRS:
I think it's going to be very useful in trying to determine which patients have greater levels of progression. So for example, you might look at a patient and you might say; Okay, this eye has mild, nonproliferative diabetic retinopathy. And then when you look specifically at the biomarkers and the change over time, you might find that these changes are progressing more rapidly in a certain cohort than others. And so this would be useful in trying to determine, say, patients at higher risk for progression. And also useful if you have some treatments that are preventing progression of retinopathy, because we can look at a more specific level, not just looking at the overall picture, but specifically at quantitative parameters, and actually quantitate the changes over time.
David Hutton:
And lastly, what are the next steps for this research?
Jennifer Lim, MD, FARVO, FASRS:
I think you know we're going to go forward and apply this to other retinal vascular diseases. We've already done this in patients with sickle cell retinopathy, and I think other diseases as well can benefit from this analysis. And I think the next step too would be to look at these changes in clinical trials patients. We can look at the changes that have happened over time, because a lot of clinical trials have images that we can look at. And we can also do this analysis based on color images, not just OCTA. So we can look at the changes, and we can see; Do our biomarkers really bear out in terms of the treatment changes? Particularly when we're giving drugs to lower the levels of NPDR. So for example, there have been anti-VEGFs that have been used to lower the level of retinopathy, say from severe to less severe forms. And we can analyze these parameters to see whether those also change, and then see over time how long the durability of these changes last, and when the parameters start changing, then we can see how helpful or non helpful the drugs were.
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.