Procedure reshapes cornea using microwave technology
A refractive procedure 15 years in the making uses microwave technology to reshape the cornea.
A refractive procedure (Keraflex, Avedro) 15 years in the making uses microwave technology to reshape the cornea. It is currently in initial clinical testing outside the United States.
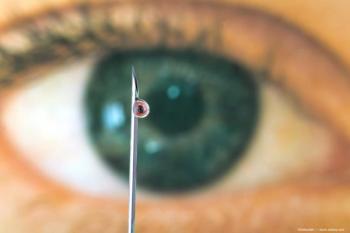
The technique changes the corneal refraction without removing stromal tissue or creating a flap. The procedure may be promising for patients with low and moderate levels of myopia who are squeamish about undergoing a conventional refractive surgery procedure in which corneal tissue is removed.
The procedure focuses microwave energy that is applied in an annular pattern to the corneal midperiphery.
Speaking to the potential market for this type of procedure, Dr. Muller said that a survey about refractive vision correction for myopia polled 2,400 consumers for specific reasons for not undergoing a refractive procedure. The top three factors cited by this group for not undergoing LASIK were "nervous about poor results," 66%; "cutting of the eye," 54%; and "fear," 45%.
The focused energy used in the procedure, delivered in one pulse of less than 100 µs, causes collagen shrinkage and corneal flattening, which does not permanently alter the cornea or require removal of corneal tissue.
The procedure is performed under the control of a microprocessor during application of electrodes to the eye. The electrodes, which can vary in thickness and the degree by which they are separated on the corneal surface, are applied to the eye outside of the visual axis.
A coolant is delivered in micropulses to control the temperature of the cornea, after which the microwave energy is applied to the cooled corneal area. The collagen in the area treated with microwave energy shrinks, which results in predictable flattening of the central cornea.
"By balancing the microwave field intensity and cooling period, the peak temperature generated can be driven to predetermined depths within the corneal stroma, causing changes in the collagen without damage to the corneal epithelium," said John Marshall, PhD, FRCPath, FRCOphth (Hon), the Frost Professor of Ophthalmology and chairman, Department of Ophthalmology, Kings College, St. Thomas' Hospital, London, and lead scientific advisor.
"Such modifications to collagen fibrils result in changes in the refractive properties of the cornea," he added. "By varying the depth and diameter of the induced collagen variations, controlled refractive changes may be introduced of different signs and magnitude. Thus, refractive errors can be corrected without removing any tissue. In vitro experiments have been conducted in both animal and human eyes using a model system capable of preserving wound healing for 4 to 6 weeks postexposure."
Histopathologic studies indicate that the induced treatment changes consist of altered collagen fibrils with modifications in the local geometry of the lamellae, Dr. Marshall said. These areas of change undergo rapid wound healing in which the matrix assumes a normal appearance and the collagen retains its newly induced curvature. A transient superficial haze apparent immediately after exposure is lost within a few minutes after treatment. By varying the administered parameters a systematic change in refraction was achieved, he said.
Marguerite B. McDonald, MD, a member of the medical advisory board and clinical associate professor of ophthalmology, Department of Ophthalmology, New York University, New York, and adjunct clinical professor of ophthalmology, Tulane University, New Orleans, commented on the procedure.
"It is early in the game vis-à-vis the clinical trials which are being conducted outside the United States. Nevertheless, the results are encouraging," she said. U.S. clinical trials are expected to begin in February 2010, with enrollment complete by January 2010.
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.