Blog: Ignore the ocular surface at your peril
Alice Epitropoulos, MD, discusses the importance of considering ocular surface health in cataract surgery patients.
Patients come in seeking
However, these efforts can be undermined by inattention to the ocular surface. The research shows that 6 to 8 of every 10 patients presenting for cataract surgery have objective signs of
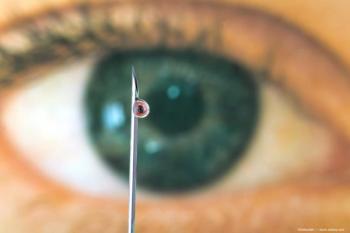
Keratometry can be dramatically affected by ocular surface disease. In 2015, several colleagues and I demonstrated that 1 out of 5 patients with hyperosmolarity experienced a refractive surprise of >1.0 D after cataract surgery, with significant variability in keratometry readings.3 It has also been shown that stabilizing the tear film preoperatively with thermal pulsation results in more accurate correction of astigmatism at the time of cataract surgery, with less residual refractive astigmatism than if the toric correction had been planned using pre-treatment keratometry.4
Dry eye can also significantly increase light scatter, reducing the clarity and stability of vision. In fact, the impact on visual quality of dry eye-related changes in the objective scatter index (OSI) measured with double-pass imaging can be as severe as that of a Grade 2-3 cataract.5 Even if the IOL power is correct, the patient may still feel that their vision is not optimal due to light scatter. This could be one key to understanding the patient who is objectively 20/20 but subjectively unhappy postoperatively.
Given the high prevalence of ocular surface disease in older populations, cataract surgeons should assume that every cataract patient has dry eye unless proven otherwise. Secondly, we should talk to the patient about this concomitant condition, what to expect, and how it can be treated. Treatment doesn’t have to be complicated and it need not result in extensive surgical delays. We have several treatments that can start improving the ocular surface in as little as 2 weeks, including perfluorohexyloctane (Miebo, Bausch + Lomb), lifitegrast (Xiidra, Novartis), thermal pulsation treatment (LipiFlow, Johnson & Johnson Vision), and even a short course of topical steroids with artificial tears. Biometry can be performed (or repeated) by staff 2-4 weeks after treatment so that the physician has accurate information on which to base the IOL calculations and surgical planning.
With these simple steps, we can ensure that patients get what they want out of cataract surgery—better vision.
References:
Trattler WB, Majmudar PA, Donnenfed ED, et al. The prospective health assessment of cataract patients’ ocular surface (PHACO) study: The effect of dry eye. Clin Ophthalmol 2017;11:1423-1430.
Gupta P, Drinkwater OJ, VanDusen KW, et al. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refract Surg 2018;44(9):1090-1096.
Epitropoulos AT, Matossian C, Berdy GJ, et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract surg 2015;41(8):1672-7.
Matossian C. Impact of thermal pulsation treatment on astigmatism management and outcomes in meibomian gland dysfunction patients undergoing cataract surgery. Clin Ophthalmol 2020;14:2283-9.
Nochez Y, Habay T, Bellicaud D, et al. Evaluation of tear film quality with a double-pass scattering index. Invest Ophthalmol Vis Sci 2011;52(14):3754.
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.