Controversy continues to surround deep sclerectomy
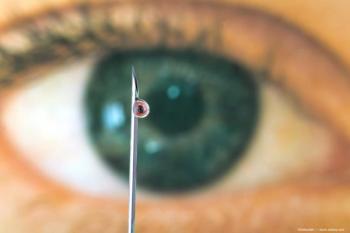
Deep sclerectomy is not the holy grail of glaucoma surgery, but available evidence indicates that it is definitively safer than trabeculectomy and that it can result in long-term success rates matching those of trabeculectomy when performed with proper technique by experienced hands, said Tarek M. Shaarawy, MD, at the World Ophthalmology Congress.
Deep sclerectomy is not the holy grail of glaucoma surgery, but available evidence indicates that it is definitively safer than trabeculectomy and that it can result in long-term success rates matching those of trabeculectomy when performed with proper technique by experienced hands, said Tarek M. Shaarawy, MD, at the World Ophthalmology Congress.
Dr. Shaarawy acknowledged that the role of deep sclerectomy in glaucoma surgery is highly controversial and that it has its drawbacks. There is a long learning curve for the procedure, each case takes more time to perform than trabeculectomy, and it is a more costly procedure as well if an implant is used. However, all publications seem to agree it has a safety advantage compared with standard filtration surgery for reducing rates of hypotony, hyphema, choroidal detachment, and particularly, surgically induced cataract.
While the efficacy of deep sclerectomy may be questioned based on the results of some studies, Dr. Shaarawy pointed out that closer examination of those reports reveals the presence of certain factors that could be expected to negatively influence the outcomes. Those potential confounders include improper depth of dissection of the deep sclera and use of Nd:YAG goniopuncture to define treatment failure.
To demonstrate the potential efficacy of deep sclerectomy, Dr. Shaarawy presented the long-term results from his own series of 105 patients in which success, defined by an IOP of 15 mm Hg or lower without medication, was achieved in 49% of eyes after up to 8 years of follow-up. About half of the eyes in the study underwent goniopuncture postoperatively, and the surgery routinely incorporated placement of a collagen implant, which Dr. Shaarawy showed in other comparative trials improved outcomes relative to deep sclerectomy without an implant.
"Deep sclerectomy is far from perfect. However, I will leave it to the able and intelligent minds of those in the audience to decide based on this information whether the take-home message is that when compared with trabeculectomy, deep sclerectomy can achieve similar IOP control with significantly fewer complications," concluded Dr. Shaarawy of Geneva, Switzerland.
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.