Collagen crosslinking shows promise for keratoconus
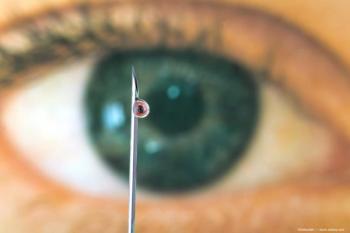
Accumulating experience with corneal collagen crosslinking indicate it is a safe and effective treatment for arresting progression of keratoconus. However, further studies are needed to better characterize its indications and contraindications.
Key Points
Results achieved with corneal collagen crosslinking for the treatment of keratoconus are very encouraging, although the technique still must be considered investigational due to a lack of sufficient data published in the peer-reviewed literature, said Theo Seiler, MD, PhD.
"In our experience, collagen crosslinking using ultraviolet A light and the photosensitizer riboflavin has been effective in stopping the progression of keratoconus in almost all eyes, and it has induced regression in about half of treated eyes based on reductions in keratometry readings," said Dr. Seiler, professor and chairman, Department of Ophthalmology, University of Zurich, and medical director, Institute for Refractive and Ophthalmic Surgery, Zurich, Switzerland. "However, we clearly need more prospective clinical data to characterize its risks and benefits and to establish a list of indications and contraindications for this procedure."
Research to date involving stress-strain measurements has shown that the collagen crosslinking procedure causes mechanical stiffening of the cornea. Corneal rigidity, as assessed by Young's modulus, increased by more than 4-fold after the procedure, Dr. Seiler said.
"The underlying mechanism for this latter effect of the crosslinking procedure is unknown, but it may play a role in the posttreatment reconstruction of the cornea," he said.
He also said his current treatment protocol for collagen crosslinking involves a partial corneal abrasion performed over a diameter of 9 mm. Then a solution of 0.1% riboflavin in 20% dextran is dropped on the cornea approximately every 3 minutes for 30 minutes. The treated cornea is irradiated for 30 minutes with a 365-nm ultraviolet light source at a distance of 5 cm using an intensity of 3 mW/cm2.
Technique alternative
"An alternative technique proposes using topical tetracaine to digest the epithelium and enable diffusion of the riboflavin into the stroma," Dr. Seiler said. "However, using confocal microscopy, we found there is keratocyte damage to a depth of about 300 to 350 μm using our crosslinking technique with corneal abrasion, whereas with the use of tetracaine, normal reflections from keratocyte nuclei can already be seen below the anterior 20 μm of stroma. Therefore, it appears there is significantly less free radical formation and crosslinking of collagen fibers using the latter technique."
He also noted that both the mechanical and biochemical effects of the procedure are very sensitive to the treatment parameters with respect to the concentration of the riboflavin solution used and the duration of application. Therefore, he encouraged that the efficacy of any modified protocol be investigated carefully prior to adoption in clinical use.
To date, Dr. Seiler and colleagues at the Technical University of Dresden, Dresden, Germany, have treated about 700 eyes with collagen crosslinking. Follow-up extending to 4 years shows the benefits are durable. An analysis including 21 patients with bilateral keratoconus who underwent crosslinking in only one eye showed the keratoconus index was increased in the untreated eyes after 1 year and significantly was higher than in the fellow crosslinked eyes.
"Crosslinking was not performed randomly in these patients but rather was used to treat the worse eye," Dr. Seiler said. "Comparisons in individual patients showed there was a significant difference in the keratoconus index between the treated and untreated eye after 1 year in nearly all patients, and the difference between eyes was highly statistically significant in some cases."
The safety profile of corneal collagen crosslinking has been favorable as well with very few complications recorded. Epithelial healing was delayed in some eyes and resulted in a subepithelial scar. More recently, in some eyes in which the procedure was repeated, a small scar in the anterior segment occurred that persisted for up to 6 months.
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.