- Ophthalmology Times, March 15 2019
- Volume 44
- Issue 5
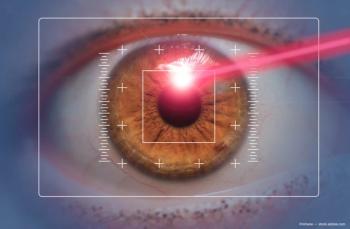
Laser refractive surgery advances expand options for myopic patients
Improving vision, nonvisual function, quality of life key for customized treatment plans
The decision of which laser refractive surgery procedure for myopia to use with a particular patient may be made by considering the benefits and limitations of each, as they pertain to particular patients, i.e., “bespoke” refractive surgery.
Reviewed by Jodhbir S. Mehta, MD, PhD
laser refractive surgery performed as LASIK, PRK, or a lenticule extraction procedure (SMILE, Carl Zeiss Meditec) can improve vision, nonvisual function, and quality of life for patients with myopia. Because of advances, each method delivers safe and effective outcomes, said Jodhbir S. Mehta, MD, PhD. Each procedure has advantages and disadvantages that may be considered in relation to patient-specific factors to guide
“We now have three great laser-based procedures to treat myopia, and that raises the question of which to choose,” said Dr. Mehta, professor and head, Corneal and External Eye Disease, Singapore National Eye Centre, Singapore. “I believe we are now in the era of what I call ‘bespoke laser refractive surgery,’ meaning that it is often patient-related factors that will determine what we do. Rather than fitting our patients to what procedure we can do, we are fitting our procedures to our patients.”
Procedure updates
A recently published paper by Dr. Mehta and colleagues reporting findings from an 18-year prospective audit of
“Comparative studies also show improvements in refractive outcomes using advanced ablation profiles, and most studies show that patients gain lines of BCVA after LASIK so that the efficacy outcomes well exceed the FDA standards,” said Dr. Mehta.
Direct comparisons of the different laser-based treatments for myopia is hampered somewhat by a relative dearth of head-to-head trials with SMILE. In one network meta-analysis that included a total of 48 randomized controlled trials, LASIK seemed to provide the best refractive outcomes. Due to advancements in excimer lasers, PRK outcomes have improved, including for the treatment of moderate to higher degrees of myopia, Dr. Mehta said.
“Compared with LASIK, PRK has advantages of a lower risk of ectasia and it avoids flap-related complications,” he said. “Slower visual recovery and risk of haze, however, remain potential drawbacks of PRK.”
While off-label application of mitomycin-C (MMC) is often used to reduce the risk of haze after PRK, MMC does not adversely affect the corneal endothelium. Some patients can experience a large drop in endothelial cell count.
“Histone deacetylase (HDAC) inhibitors, which are FDA-approved for treatment of hematologic cancers, have anti-fibrotic activity. In an experimental model, we found that an HDAC inhibitor was effective for mitigating corneal haze after PRK,” he said, adding results showed it was as effective as MMC with the potential for better short- and long-term safety.
The functional results after SMILE seems comparable to those achieved with the excimer laser procedures, but the lack of automated centration remains an issue with SMILE. Maintaining centration and reducing the energy of the laser when creating the lenticule improves SMILE outcomes.
He considers several “bespoke features” when deciding which laser refractive surgery is best for a patient seeking myopia correction. Because of the long time needed to create the lenticule, he excludes SMILE if a patient seems nervous or is likely to be uncooperative.
SMILE, PRK over LASIK
As flapless procedures,
Other bespoke features he considers include:
- Presence of dry eye-patients at risk of dry eye preoperatively may be more suited to PRK and SMILE than LASIK
- Desire for rapid visual recovery-LASIK gives the fastest visual recovery followed by SMILE and then PRK
- Level of preoperative HOA-high levels of HOA can be treated with a topography-guided ablation that is currently only available with LASIK and PRK.
Disclosures:
Jodhbir S. Mehta, MD, PhD This article is based on a presentation given by Dr. Mehta at the 2018 Refractive Surgery Subspecialty Day meeting. He receives lecture fees and grant support from Carl Zeiss Meditec and Ziemer.
Articles in this issue
almost 7 years ago
Valuing power of the lenticlealmost 7 years ago
CAIRS may eliminate complications from synthetic ring segmentsalmost 7 years ago
Long-term data establish SMILE role in myopic treatment armamentariumalmost 7 years ago
Hydrophilicity RIS setting stage as new paradigm for refractive surgeryalmost 7 years ago
2019: State of corneal crosslinking for patients with keratoconusalmost 7 years ago
Study: RLE, monovision LASIK results similar in 45-60 age groupalmost 7 years ago
Pearls for building the corneal inlay patient base in your practicealmost 7 years ago
Making the most of diagnostic technology toolkitalmost 7 years ago
Optical sector must embrace the telemedicine waveNewsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.